Men with fertility issues
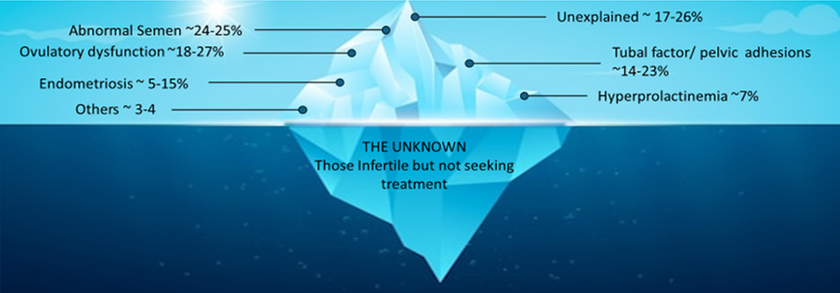
It is estimated that 25% of infertility is due to abnormalities in the male partner. At MFS, we offer expert diagnosis and treatment for male infertility.
Our care for men facing fertility issues includes the following benefits:
A comprehensive fertility clinic providing solutions for all your fertility needs in one convenient location
Our on-site services are available Monday to Friday every week.
MFS collaborates with a board-certified male fertility urologist and a CLIA-certified laboratory director
Normal sperm count equals or exceeds 15 million sperm per milliliter (mil/mL) of semen. At MFS, when sperm concentrations are < 10 million/mL or there are abnormal sexual functions or findings suggestive of endocrinopathy, we perform endocrine evaluations to elucidate the hormonal causes of male infertility. Evaluation includes physical examination, scrotal and prostate ultrasound, and endocrine and genetic testing to discover the cause of the problem. An appropriate individualized treatment plan is then recommended.
Awonuga A., Camp, O. G., Biernat, M. M, & Abu-Soud, H. M. (2025). Overview of infertility. Systems Biology in Reproductive Medicine, 71(1), 116–142. PMID: 40117219.
Evaluation of male fertility
Necessary investigations include measuring serum Follicle stimulating hormone (FSH), Luteinizing hormone (LH), Estradiol (E), Prolactin (PrL), Thyroid stimulating hormone (TSH), Vitamin D (Vit D), Testosterone (T) performed in the early morning (8 AM to 10 AM), and serum hormone binding globulin (SHBG). When serum T is low, we often repeat the test because, like in women, they are secreted in a pulsatile fashion. Normal FSH levels (≤ 7.6 IU/L) suggest normal sperm production (spermatogenesis); elevated FSH levels indicate abnormal spermatogenesis (the process by which sperm cell production occurs).
When sperm concentrations are < 5 million/mL (severe oligospermia), especially with associated low T, high FSH, and LH, and those with nonobstructive azoospermia (no sperm in the ejaculate not due to obstruction of the tubes taking sperm from the testis to the penis), such as those with primary hypogonadotropic hypogonadism (HH) should have chromosomal evaluation to exclude chromosomal microdeletions on the Y chromosomes, translocations, inversions, duplication, mosaics, and extra X chromosomes (Klinefelter syndrome 47, XXY). For successful treatment outcomes, patients with severe oligospermia require extensive counseling, in vitro fertilization (IVF)/intracytoplasmic sperm injection (ICSI), and preimplantation genetic testing for aneuploidy (PGT-A), monogenic disease (PGT-M), and structural rearrangement (PGT-ST).

Sperm DNA fragmentation testing
MFS’s fertility specialists conduct a thorough clinical evaluation with state-of-the-art semen analysis. This analysis involves a trial gradient sperm wash to assess the feasibility of fertility treatments such as intrauterine insemination (IUI) and In-vitro fertilization (IVF) with intracytoplasmic sperm injection (ICSI).
In cases of a varicocele, fertilization failure, poor embryo development after IVF, or recurrent pregnancy loss we recommend that men undergo assessment of sperm DNA fragmentation. Sperm DNA fragmentation testing assesses the level of damage or fragmentation in the DNA of sperm cells, which can indicate the quality of a person's sperm and may affect fertility. The test involves analyzing a semen sample to determine the DNA fragmentation index (DFI), the percentage of sperm with fragmented DNA, which may inform a recommendation for the type of treatment to offer couples.
The performance of sperm DNA fragmentation will be done at the C.S. Mott Center for Human Growth and Development at Wayne State University in a CLIA-certified laboratory for advanced analysis of male infertility.
Treatments
Men with varicoceles
Although some advocate surgery, no clinical trial evidence has shown that surgical treatment improves fertility.
Men with oligospermia
Sperm concentration below 5 mil/mL is designated severe. At MFS, for men with severe oligospermia, we take blood to measure their Testosterone (T)/Estradiol (E) ratio after excluding chromosomal causes to determine what medication to use to improve sperm count, particularly in those who cannot afford IVF. Testosterone and estradiol levels must be within normal ranges to calculate the ratio. Normal sex hormone levels and T/E2 ratios < 10, i.e., those with a Low T/E2 ratio, are treated with aromatase inhibitors like anastrozole or Letrozole for 6 months, with repeat semen analysis (SA) in 3 months. Therefore, an increase in E2 hormone, hence a T/E2 level, i.e., 10 are treated with Clomiphene Citrate (Clomid) for 6 months and have repeat SA in 3 months. These medications are not recommended in hypergonadotropic (high FSH and LH) males due to the severity of testicular damage. Therefore, the patient should have normal gonadotropins, hence be normogonadotropic.
Men with low sperm count
For men with low motile sperm counts below the range of 1 to 5 million, IVF with ICSI is the treatment of choice. Despite the increased use of ICSI to ensure against fertilization failure, a cohort study of more than 300,000 IVF cycles showed lower rates of implantation and live birth when ICSI was performed for indications other than severe male infertility. MFS’s fertility specialists conduct a thorough clinical evaluation with state-of-the-art semen analysis. This analysis involves a trial gradient sperm wash to assess the feasibility of fertility treatments such as intrauterine insemination (IUI) and In-vitro fertilization (IVF) with intracytoplasmic sperm injection (ICSI).
Men who do not have sperm in their ejaculate (Men with azoospermia)
Some men do not have sperm in their ejaculate (termed azoospermia) because of obstruction in the tubes that transport sperm to the urethral opening, while some have reduced sperm or no sperm production from the testicles. Some men do produce sperm but instead of the sperm reaching the penis it is retro gated into the bladder. This may be due to retrograde ejaculation that can be treated by using medications to help close the bladder neck or by retrieving the urine, processing it, and using it for artificial insemination or other assisted reproductive techniques. Once retrograde ejaculation is excluded, others will need sperm to be retrieved from the epididymis (convoluted tubes behind the testis in men carry sperm from the testis when produced) or the testis. Sperm retrieval techniques are named depending on the method used and the source of the sperm. Examples are: 1.Epididymal sperm aspiration (ESA): Involves aspiration of sperm with a fine needle from the epididymis. This can be done by inserting a fine needle through the skin under local anesthesia in a process called percutaneous epididymal sperm aspiration (PESA), or an operating microscope is used to locate and aspirate sperm from the epididymal tubes in a process called microsurgical epididymal sperm aspiration (MESA) 2.Testicular Sperm Aspiration (TESA). In TESA, sperm is retrieved directly from the testicles using a fine needle, unlike its counterpart, TESE, which involves biopsy of the testicular tissue. 3.MicroTESE involves making small testicular incisions and using a microscope to locate and extract sperm-producing tissue. It should be noted that sperm retrieved by TESA and MESA can only be used in assisted reproductive technologies like IVF, often combined with intracytoplasmic sperm injection (ICSI)
An online calculator for calculating T/E2 levels can be found here.
Our Story
Since 1992, Dr. Awonuga has been helping couples and women achieve their dream of taking a baby home following infertility treatment. Once practiced as Division and Fellowship Program Director at Wayne State University/Wayne Health Reproductive Endocrinology and Infertility practice, he has now opened Michigan Fertility Services. Dr. Awonuga is an active researcher and continues to collaborate with scientists at the C.S. Mott Center for Human Growth and Development at Wayne State University. With extensive experience in the field, at Michigan Fertility Services we will educate our patients and be gentle, ethical, and respectful. These are essential because as inability to conceive and have children is associated with anxiety and psychological stress. Dr. Awonuga understands and will help manage these facets with an appropriate referral if necessary.
